Credit to Mr. Dinkov for his exposure of this topic for me. This article is a combination of his words and mine with expansion on figures and other aspects of ODSFA and BCFAs by myself.
http://haidut.me/
Odd-chain saturated fatty acids are fatty acids with an odd number of carbon atoms and no double bonds. From here on, I will refer to the odd-chain saturated fatty acids as ODSFA. The most common ODSFA are the saturated C15 and C17 derivatives, respectively pentadecanoic acid and heptadecanoic acid. The ODSFAs have been only occasionally researched but recent interest has come from large longitudinal studies dubbing a phenomenon called the “Full Fat Paradox” or “Dairy Fat Paradox.”
A recent meta-analysis including over 20 cohort studies suggests an inverse association of whole and low fat dairy with incidence of type II diabetes, however, no significant associations were found for high fat dairy. This meta-analysis, alongside other studies, has called into question the previous consensus about the health value of reduced fat milks, as an universal prescription.
Odd-chain fatty acids are present in milk and there's evidence that pentadecanoic(C15:0) and heptadecanoic(C17:0) acids are present in many foods' fat in proportions equivalent to dairy. These foods include fish, seaweed, and even vegetables- though obviously the vegetables are not a great source due to low fat content- the amount of BCFA can be altered(increased) by fermentation, though levels remain low.
Here are two links to foods sorted by their content of C15:0 and C17:0
One quart of whole milk is 976 grams at 3.25% fat(in the US)- this means ~32 grams of fat. This would come out to ~390 mg of C15:0 and ~195mg of C17:0. This meets the upper-range and then some for recommended C15:0 intake. C17:0 is established as a PPARδ agonist and PPARδ agonism via aspirin was connected to the amelioration of NAFLD- more generally, PPARδ is connected to general metabolic wellbeing. C15:0 is an established PPARδ and PPARα agonist, as well.
In addition to the ODSFA, I would draw attention to the branched-chain fatty acids and long-chain fatty acids. These fatty acids are getting some attention and there's a growing body of research to suggest positive effects. Georgi Dinkov(known as @haidut on twitter) has collected a study here. I would also add his Ray Peat forum post for DeFibron- which contains methyl saturated fatty acids(a subject on later writing in this blog, especially for their potential role in cytoplasmic stability) on account of their role in preventing liver fibrosis, inflammation, and increasing endotoxin resistance.
BCFAs are anti-endotoxin and are incorporated preferentially by bacteria like Staph into their endotoxins which reduces TLR2 activation by reduced immunostimulation and allowance of endotoxin "inactivation" by common lipases.
Staph incorporate unsaturated fatty acids(UFA) over BCFA if they cannot produce BCFA themselves due to resource scarcity or demand for lipid synthesis is high. This flexibility in the Staph fats gives rise to the possibility for increased numbers of antimicrobial-resistant Staph- facilitated by diets rich in unsaturated fatty acids, specifically linoleic acid and arachidonic acid.
The positive effects of the odd-chain fatty acids is partially mediated by the effects on endotoxin and I’d like to show you(the reader) more data and studies on the effects of odd-chain fatty acids on health. One area of effect from the ODSFAs that provides clues into the mechanism of health comes from some Japanese studies(1 and 2) looking at the impact of pentadecanoic acid on hair follicles. One of the studies is in Japanese and as such required far too long with google translate and a medical/biochemical kanji dictionary. Either way, the odd-chain fatty acids, due to their saturated nature and their odd number of carbons, are not metabolized in the same way as even-number carbon fats.
Pentadecanoic acid is only partially metabolized via the beta-oxidation pathway, through which even-chain fatty acids get metabolized to ultimate form acetyl-CoA and then enter the Krebs Cycle. The terminal metabolism of odd-chain fatty acids, including pentadecanoic acid, forms succinic acid, and ultimately succinyl-CoA, which then enters the Krebs Cycle.
The rising levels of acetyl-CoA has an inhibitory effects on pyruvate dehydrogenase (PDH). As such, eating a diet high in fat with mostly even-chain fats would result in reduction of glucose metabolism, even if all the fats are of the SFA type.
However, if those fats are of the odd-chain species and enter the Krebs Cycle as succinic acid, then virtually no such reduction of glucose metabolism is expected to occur and, in fact, pentadecanoic acid was described in the Japanese studies as stimulating mitochondrial function and ATP production, which ultimately resulted in improved hair growth. This improved ATP production and mitochondrial function are directly related to improved oxidative phosphorylation.
The Japanese researchers filed a patent for treating hair-loss with pentadecanoic acid and in that patent they stated the possibility for other odd-chain fatty acids with similar length, especially the C17:0 heptadecanoic acid mentioned above, would have similarly beneficial effects on hair-growth through increasing oxidative phosphorylation.
The effects of the dairy fats and ODSFAS continues with a comprehensive study on the Pentadecanoic and Heptadecanoic acids. This study also discussed the role of the ODSFAs on mitochondria and metabolic health. I have included a large selection of quotes from the study to show this.
“…The robust inverse association of 15:0 and/or 17:0 concentrations in plasma phospholipids or RBCs with cardiovascular disease (CVD) and type 2 diabetes mellitus (T2D) risk is quite impressive… They may be used for synthesis of odd-numbered VLCFAs, provide anaplerotic intermediates for the CAC, or store away excess propionic acid. ”
Another study of the paradoxes found “…Further, an 18-year longitudinal study including over 25,000 individuals demonstrated that children fed whole fat milk had a lower risk of having obesity compared to children who were provided fat-free or 1% fat milk, and multiple studies have demonstrated associations between higher dietary intake of full-fat dairy and reduced risk of type 2 diabetes and cardiovascular disease. As such, there is a need re-evaluate potential health risks versus benefits of dietary dairy fats.”
Additionally, the authors found “…While dietary ECFAs have been associated with increased risk of inflammation, heart disease, and type 2 diabetes in humans, higher dietary intake and circulating levels of OCFAs have been associated with lower risks of adiposity, chronic inflammation, cardiovascular disease, metabolic syndrome, type 2 diabetes, nonalcoholic steatohepatitis (NASH), chronic obstructive pulmonary disease, pancreatic cancer and other conditions. In a prospective cohort involving over 14,000 people followed for an average of 14 years, increased dietary intake of OCFAs was associated with lower mortality in both men and women, while higher ECFA intake was associated with higher mortality in women.”
“…Since fatty acids can affect mitochondrial function, the effects of OCFAs and ECFAs on repairing mitochondrial function and reducing mitochondrial ROS were evaluated in serum starved HepG2 cells. Here, C15:0 had a dose-response u-curve effect on mitochondrial function, including lower mitochondrial ROS production in cell systems supplemented at 10 µM (17.8 ± 2.7%, P = 0.04), 20 µM (12.9 ± 3.2%, P = 0.005) and 50 µM (15.4 ± 2.6%, P = 0.007) compared to non-supplemented control cell systems (23.4 ± 4.3%) (Fig. 1). There were no differences in ROS production when comparing cells supplemented at higher C15:0 concentrations (100 and 200 µM) compared to non-supplemented controls. Among a variety of other OCFAs and ECFAs evaluated (C13:0 through C18:0), C15:0 through C18:0 (20 µM) had lower mitochondrial ROS compared to the non-supplemented control group, while C13:0 and C14:0 did not significantly lower mitochondrial ROS (Suppl Fig. 2).”
“…Based on a definition of cytotoxicity in which more than 50% of total protein in the cell system was reduced, C15:0 did not induce cytotoxicity in any of the 12 cell systems (Suppl Table 2).”
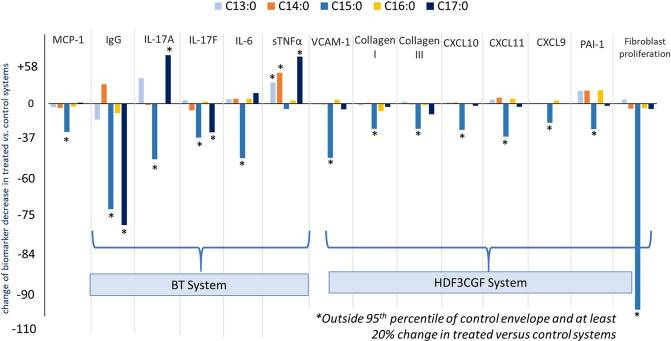
“…Here, C15:0 had dose-dependent, annotated anti-inflammatory activities, including reduced monocyte chemoattractant protein 1 (MCP-1) and secreted immunoglobulin G (IgG) (Fig. 2). C15:0 also had antifibrotic activities, including reduced Collagen I, plasminogen activation inhibitor 1 (PAI-1), and 72-hour fibroblast proliferation (Fig. 2)…. C15:0 cell-based anti-inflammatory and antifibrotic activities at 20 µM were better than C17:0 at the same concentration; other saturated fatty acids (C13:0, C14:0 and C16:0) had no anti-inflammatory or antifibrotic activities (Fig. 3). Because C14:0, C15:0, and C16:0 all had similar dual PPARα/δ agonist activities (reported above), results from our human cell phenotypic screening support that C15:0 activities go beyond C15:0’s role as a natural PPARα/δ fatty acid ligand. This study also supports that a relatively minor increase in C15:0 concentrations (e.g. from 2.2 µM to 6.7 µM) can positively impact its anti-inflammatory and antifibrotic activities.”
Fig. 2
Fig. 3
“…Thus, a single oral dose of C15:0 at 35 mg/kg succeeded in achieving our targeted active plasma concentrations in this rodent model, between 2.5 to 5 µg/ml (equivalent to 6.7 to 20 µM), from 1 to 8 hours post-dose. Plasma total C17:0 levels also increased, albeit less so than C15:0, following a single oral dose of C15:0; similar, sustained increases were not apparent with C13:0 (Fig. 4). These findings support de novo elongation of C15:0 to C17:0.”
“…These levels are consistent with our studies, which demonstrated cell-based PPARα/δ agonist, anti-inflammatory, antifibrotic, and mitochondrial protective C15:0 activities between 10 and 50 µM, with most of our studies demonstrating optimal activities at 20 µM. Human pharmacokinetic studies support that a single dose of 200 mg of C15:0 results in 20 µM circulating C15:0 concentrations (approximately 5 µg/ml)”
“…To further evaluate the safety of C15:0 at increasing doses, Sprague Dawley rats (n = 10 per group, 5 females and 5 males, 7 to 8 weeks old) were dosed orally once daily for 14 days with C15:0 at 35, 175 and 350 mg/kg body weight. A non-dosed vehicle control group was included. Safety assessments included clinical observations, body weight, food intake, clinical chemistries, and histology (liver, kidney, heart, and adrenal glands). Additionally, total plasma C15:0 and C17:0 concentrations were measured at Day 14. There were no mortalities or observed abnormal behaviors in animals throughout the 14-day study across all study groups, and there were no significant differences when comparing body weights and organ weight-to-body weight ratios or the prevalence of abnormal clinical chemistry values or histologic observations between C15:0-supplemented and non-supplemented control animals (Suppl Table 3). ”
“…Mice supplemented with oral C15:0 for 90 days at low doses (5 mg/kg) had lower circulating levels of the proinflammatory chemokine, monocyte chemoattractant protein 1 (MCP-1), and the proinflammatory cytokine, interleukin 6 (IL-6) compared to non-supplemented controls (Fig. 5). The C15:0-supplemented group also had lower glucose, lower cholesterol, and lower percent body weight gain on the high fat diet compared to non-supplemented controls (Fig. 5, Suppl Table 4). In contrast, mice supplemented with daily low dose C17:0 (5 mg/kg) had no significant differences in clinical chemistry values compared to non-supplemented, diseased controls, while high dose C17:0 (50 mg/kg) supplemented mice had lower serum MCP-1 compared to controls (Suppl Table 4). ”
“…Specifically, C15:0 supplementation raised hemoglobin, hematocrit, and red blood cell count, and lowered nucleated red blood cells, red blood cell distribution width, and reticulocytes. In this model, these changes are consistent with decreased loss of fragile red blood cells and lowered need for new red blood cell production. Further, C15:0-supplemented animals had lower cholesterol, triglycerides, globulins, and platelets compared to non-supplemented diseased controls (Fig. 7). Additionally, multiple liver health indices in C15:0-supplemented animals, including bilirubin and icterus were lower than non-supplemented diseased controls, matching that of healthy controls (Supplement Table 6). Histologically, C15:0-supplemented animals also had less severe liver fibrosis and liver iron staining scores within Kupffer cells compared to non-supplemented diseased controls. Unlike the non-supplemented diseased controls, C15:0-supplemented animals did not progress from Stage 2 to Stage 3 (bridging) fibrosis (Suppl Table 6).”
“…Here, we show C15:0 as an active dietary fatty acid that attenuates inflammation, anemia, dyslipidemia, and fibrosis in vivo, potentially by binding to key metabolic regulators and repairing mitochondrial function. This is the first demonstration of C15:0’s direct role in attenuating multiple comorbidities using relevant physiological mechanisms at established circulating concentrations. Pairing our findings with evidence that (1) C15:0 is not readily made endogenously, (2) lower C15:0 dietary intake and blood concentrations are associated with higher mortality and a poorer physiological state, and (3) C15:0 has demonstrated activities and efficacy that parallel associated health benefits in humans, we propose C15:0 as a potential essential fatty acid. Further studies are needed to evaluate the potential impact of decades of reduced intake of OCFA-containing foods as contributors to C15:0 deficiencies and susceptibilities to chronic disease.”
The wide-spread effects of C15:0(pentadecanoic acid) extend beyond effects on inflammation and metabolism on blood cells or aggregate populations. C15:0 is becoming considered a true candidate for an “essential” fatty acid due to its demonstrated effects. Additionally, pentadecanoic acid has been shown to have effects on the brain and mental health.
“…A growing body of evidence supports that pentadecanoic acid (C15:0), an odd-chain saturated fat found in butter, is an essential fatty acid that is necessary in the diet to support long-term metabolic and heart health. Here, dose dependent and clinically relevant cell-based activities of pure C15:0 (FA15TM) were compared to eicosapentaenoic acid (EPA), a leading omega-3 fatty acid, as well as to an additional 4,500 compounds. These studies included 148 clinically relevant biomarkers measured across 12 primary human cell systems, mimicking various disease states, that were treated with C15:0 at four different concentrations (1.9 to 50 μM) and compared to non-treated control systems. C15:0 was non-cytotoxic at all concentrations and had dose dependent, broad anti-inflammatory and antiproliferative activities involving 36 biomarkers across 10 systems. In contrast, EPA was cytotoxic to four cell systems at 50 μM. While 12 clinically relevant activities were shared between C15:0 and EPA at 17 μM, C15:0 had an additional 28 clinically relevant activities, especially anti-inflammatory, that were not present in EPA. Further, at 1.9 and 5.6 μM, C15:0 had cell-based properties similar to bupropion (Pearson’s scores of 0.78), a compound commonly used to treat depression and other mood disorders. At 5.6 μM, C15:0 mimicked two antimicrobials, climabazole and clarithromycin (Pearson’s scores of 0.76 and 0.75, respectively), and at 50 μM, C15:0 activities matched that of two common anti-cancer therapeutics, gemcitabine and paclitaxel (Pearson’s scores of 0.77 and 0.74, respectively). In summary, C15:0 had dose-dependent and clinically relevant activities across numerous human cell-based systems that were broader and safer than EPA, and C15:0 activities paralleled common therapeutics for mood disorders, microbial infections, and cancer. These studies further support the emerging role of C15:0 as an essential fatty acid.”
“…When assessing clinically relevant and dose-dependent activities of C15:0 and over 4,500 additional compounds, our study demonstrated common cell-based phenotypic profiles between C15:0 and therapeutics for mood disorders, infections, and cancer, based on concentration. At lower concentrations (1.9 and 5.6 μM), C15:0 human cell-based activities closely matched those of bupropion at 10 and 30 μM, respectively. Bupropion, sold as Wellbutrin®, is a dopamine-norepinephrine reuptake inhibitor and commonly used antidepressant that is considered safe, well tolerated, and does not result in weight gain [51]. Specific conditions managed by bupropion include major depressive disorder and seasonal affective disorder, and it has shown promise as a non-nicotine agent that promotes smoking cessation in clinical trials [51]. Bupropion is a pill that is typically taken 2–3 times a day in doses ranging from 100–150 milligrams. Based on human pharmacokinetic data with pure free fatty acid C15:0, approximate doses of 19 to 56 mg is expected to achieve circulating C15:0 concentrations with activities similar to bupropion[52].”
Readers of this blog should address my comments in my article on the Omega-9 fatty acids wherein I give some brief comments regarding the potential negative effects of the omega-3 fatty acids. In the above study, the study used EPA(an omega-3 acid) and, predictably, the EPA exposure was not associated with improved outcomes. EPA has 5 double bonds, in contrast to DHA’s 6, so this would indicate a high degree of potential damage due to oxidation risk.
The ODSFAs are also being considered as “a potential adjuvant therapy for lung cancer (NSCLC).” This is due to the fact that the odd-chain saturated fatty acid (OCSFA), heptadecanoic acid (C17:0), profoundly inhibits non-small-cell lung cancer (NSCLC) cell proliferation.”
An indication that the ODSFAs can hold immense medical benefits stems from the efficacy of the ODSFAs to improve the health and wellbeing on non-human species, like dolphins.
Per capita intake estimates say that Americans consume ~400-500mg BCFAs daily, however, dairy product and milk consumption are not normally-distributed, so a per-capita intake is not an exact depiction of what the average or median American is really eating.
Personally, I wouldn't be surprised if BCFA intake by most Americans was half of this amount, especially amongst vegetarians and vegans and Gen Z(the latter are the lowest milk and dairy consuming generation in US history). Additionally, there is pervasive stigma in the Gen Z community with 49% describing shame at ordering dairy in front of peers.
For reference:
"Our data indicate that BCFA intake can exceed the estimated per capita consumption of 492 mg/d by at least two-fold with common intakes of popular foods. For example, daily consumption of 150 g (5.3 oz) of cooked ground beef (18% fat, with 1.8%wt BCFA on average), two cups (473 ml) of whole milk (3.25%fat, 2%wt BCFA), and 57 g (2 oz) of cow’s milk-based cheese (25% fat, 1.8%wt BCFA on average) contains about 1050 mg BCFA. If the cows’ milk cheese was replaced with sheep cheese (31% fat and 2.7%wt BCFA), then the meal BCFA would exceed 1700 mg BCFA, or three fold the average intake."
150g of cooked ground beef at ~85% lean, 2 cups of whole milk, and 2oz cheddar cheese is 65g of protein and 56g of fat(1.3g omega-6) on Cronometer, btw.
To summarize, there are many reasons why dairy products are tied to health and well-being- part of this is the numerous and healthful saturated fatty acids. A quart a day keeps the doctor away! Be sure to eat your seafood and your ruminant meat too!